What is Single Embryos Transfer? Is it more effective?
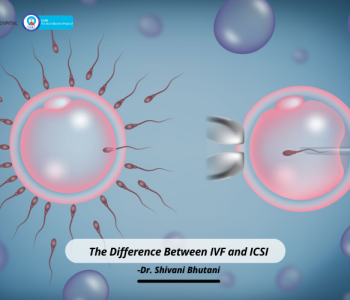
 IVF and ICSI
IVF and ICSI
What is Single Embryos Transfer? Is it more effective?
Most women going for IVF treatment are typically told that multiple-embryo transfer improves their chances of having a successful pregnancy within the desired outcome. When it is impressed upon them that multiple-embryo transfer is less likely to require a second transfer, couples undergoing this treatment are more than keen to go for this plan which means the treatment would be a lot more affordable than going for a single embryo transfer.
However, choosing between multiple embryo transfer and single embryo transfer is a decision that must be made after thoroughly considering the various aspects of these two options. Before we proceed with that, it makes sense to first be aware of what a single or multiple embryo transfers means.
What is embryo transfer?
An embryo transfer is the last part of the IVF process. Once your eggs have been fertilized, they are cultured for 1-2 days. The best embryo is then chosen to be transferred to the woman’s uterus for development.
In the initial days of IVF, fertility experts relied on transferring multiple embryos to boost success rates. With time and advancement in technology, reproductive experts can now identify one embryo with better pregnancy success and transfer a single one into the uterus. This is done with the assistance of new-age technologies such as extended embryo culture, time-lapse photography, and preimplantation genetic testing for aneuploidy (PGT-A) and vitrification.
Single versus multiple embryos transfer: Which one to choose?
A study conducted in 2010 by lead researchers DJ McLemon at the University of Aberdeen in Scotland revealed that women undergoing in-vitro fertilization treatment are nearly five times more likely to carry a baby to term if they undergo a single embryo transfer instead of a double embryo transfer. Experts also point out that when a healthy embryo is placed alongside a poor-quality embryo, the body as its natural tendency would focus more on the poor-quality embryo than the healthy one. This would cut down the chances of pregnancy.
Several studies conducted on the subject argue that the success rate of IVF does not depend on the number of embryos that are transferred but on the quality of the selected embryo. Newer research has also pointed out that success rates are equal for women transferring a single PGS-tested embryo and women transferring multiple non-PGS-tested embryos.
Modern researchers are also of the opinion that doctors should recommend single embryo transfer to women undergoing IVF treatment.
Benefits of single embryos transfer
- Reduced complications associated with multiple pregnancies.
- Lower risk of perinatal illness.
- Lower risk of maternal illness.
- Lower risk of death in childbirth.
- Lower healthcare costs of delivering.
Risks with multiple embryos transfer
Some of the most common risks associated with multiple embryo transfers is the risk of multiple pregnancies. Not only is this highly risky for both the mother and the children, but also an undesired outcome for many couples.
Data show that the multiple birth rate in Australia and New Zealand decreased from 7.9% in 2010 to 2.9% in 2019. This improvement was driven by the increased proportion of IVF cycles where only a single embryo is transferred, up from 70% in 2010 to 92% in 2019.
Data also show that in the case of multiple pregnancies, the risk of labor complications and infant mortality shoots up. Premature birth and low-birth weight are some other problems in case of multiple pregnancies. Because of these reasons, for instance, single embryo transfer is the most seriously considered option in Sweden today.
However, the multiple-embryo transfer tends to benefit older patients more than it benefits younger patients.
Who is the right candidate for single embryo transfer?
- Women aged up to 35 years
- Women undergoing their first ART cycle
- Women who had a successful pregnancy in a previous ART cycle
- Women with a relatively large number of high-quality embryos
- Women having embryos available for freezing to use in a later cycle